eISSN 2444-7986
DOI: https://doi.org/10.14201/orl.29465
REVIEW
PATHOLOGICAL UPTAKE WITH 18-FLUOROCHOLINE VERSUS 99mTc-MIBI IN THE LOCATION OF THE PARATHYROID GLANDS IN HYPERPARATHYROIDISM. SYSTEMATIC REVIEW AND META-ANALYSIS
Captación patológica con 18-Fluorocolina frente a 99mTc-MIBI en la localización de las glándulas paratiroides en el hiperparatiroidismo. Revisión sistemática y metanálisis
José Luis PARDAL REFOYO 1  , Pilar TAMAYO ALONSO 2
, Pilar TAMAYO ALONSO 2  , Sofía FERREIRA CENDÓN 1
, Sofía FERREIRA CENDÓN 1  , Esther MARTÍN GÓMEZ 2
, Esther MARTÍN GÓMEZ 2 
1University Hospital of Salamanca, Salamanca.
2University Hospital of Salamanca, Salamanca. Biomedical Research Institute (IBSAL). Nuclear Medicine
Correspondencia: jlpardal@usal.es
Reception date: June 9, 2022
Date of Acceptance: July 19, 2022
Publication date: July 22, 2022
Date of publication of the issue: March 25, 2024
Conflict of interest: The authors declare no conflicts of interest
Images: The authors declare that the images have been obtained with the permission of the patients
Rights policy and self-archive: the self-archive of the post-print version (SHERPA / RoMEO) is allowed
License CC BY-NC-ND. Creative Commons Attribution-Noncommercial-NoDerivate Works 4.0 International
University of Salamanca. Its commercialization is subject to the permission of the publisher
SUMMARY: Introduction: The location of the pathological parathyroid glands in hyperparathyroidism is usually carried out by means of 99mTc-sestamibi scintigraphy, which increases its precision by adding the ultrasound examination. The non-localization of the parathyroid glands increases the difficulties for surgical removal. To increase the detection of pathological glands, other radioactive tracers are used, such as methionine, fluorocholine or 18F-flurpiridaz.
Objective: To establish if PET / CT with 18-Fluorocholine in patients with hyperparathyroidism increases the number of uptakes compared to the 99mTc-sestamibi scan.
Method: Systematic review and meta-analysis. Two subgroups were analyzed. Subgroup 1: trials comparing both techniques as an initial exploration. Thirteen studies including 1131 examinations were selected (596 PET / CT with 18-Fluorocholine vs. 535 scintigraphy with 99mTc-sestamibi). Meta-analysis was performed following the random effects model and the odds ratio was calculated. Subgroup 2: studies that include 18-Fluorocholine as a rescue examination in patients with a previous negative study with a 99mTc-sestamibi scan. 17 articles including 412 examinations with 359 patients in which there was at least one uptake were selected. Meta-analysis of the prevalence of the number of patients in whom there was at least one uptake was performed using the random effects model.
Results: Subgroup 1: The number of patients in which at least one uptake occurs is significantly higher with the 18-Fluorocholine examinations (OR 4.264, 95% CI 2.400-7.577). The prevalence of uptake with 18-Fluorocholine is 0.91 [0.86, 0.95] and with sestamibi 0.68 [0.56, 0.80]. Subgroup 2: the prevalence of uptake among patients with previous negative MIBI studies was 0.90 [0.87, 0.94]. The probability of detection of both techniques in this group reaches 0.98. Publication bias in the meta-analyzes is low.
Discussion: 18-Fluorocholine protocols provide higher precision, clearer images, with faster acquisition as well as being readily available for most PET / CT centers.
Conclusion: The PET / CT study with 18-Fluorocholine can be recommended as a study for the location of pathological parathyroid glands after studies with negative MIBI.
KEYWORDS: Hyperparathyroidism; parathyroid; sestamibi scintigraphy; choline PET; fluorocholine
RESUMEN: Introducción: La localización de las glándulas paratiroides patológicas en el hiperparatiroidismo usualmente se realiza mediante gammagrafía con 99mTc-sestamibi que incrementa su precisión al añadir la exploración ecográfica. La no localización de las glándulas paratiroides incrementa las dificultades para la extirpación quirúrgica. Para incrementar la detección de glándulas patológicas se utilizan otros trazadores radiactivos como la metionina, la fluorocolina o el 18F-flurpiridaz.
Objetivo: Establecer si el PET/TC con 18-Fluorocolina en pacientes con hiperparatiroidismo incrementa el número captaciones comparada con la gammagrafía con 99mTc-sestamibi.
Método: Revisión sistemática y metanálisis. Se analizaron dos subgrupos. Subgrupo 1: ensayos que comparan ambas técnicas como exploración inicial. Se seleccionaron 13 estudios que incluyen 1131 exploraciones (596 PET/TC con 18-Fluorocolina vs. 535 gammagrafía con 99mTc-sestamibi). Se realizó metanálisis siguiendo el modelo de efectos aleatorios y se calculó la odds ratio. Subgrupo 2: estudios que incluyen la 18-Fluorocolina como exploración de rescate en pacientes con estudio previo negativo con gammagrafía con 99mTc-sestamibi. Se seleccionaron 17 artículos que incluyen 412 exploraciones con 359 pacientes en los que al menos hubo una captación. Se realizó metanálisis de la prevalencia del número de pacientes en los que hubo al menos una captación aplicando el modelo de efectos aleatorios.
Resultados: Subgrupo 1: El número de pacientes en los que se presenta al menos una captación es significativamente superior con las exploraciones con 18-Fluorocolina (OR 4.264, IC 95% 2.400-7.577). La prevalencia de captaciones con 18-Fluorocolina es de 0.91 [0.86, 0.95] y con sestamibi de 0.68 [0.56, 0.80]. Subgrupo 2: la prevalencia de captaciones entre pacientes con estudios MIBI negativos previos fue de 0.90 [0.87, 0.94]. La probabilidad de detección de ambas técnicas en este grupo llega al 0,98 El sesgo de publicación en los metanálisis es bajo.
Discusión: Los protocolos con 18-Fluorocolina proporcionan mayor precisión, imágenes más claras, con una adquisición más rápida además de estar fácilmente disponible para la mayoría de los centros PET / CT.
Conclusión: El estudio PET/TC con 18-Fluorocolina puede recomendarse como estudio para la localización de las glándulas paratiroides patológicas tras estudios con MIBI negativos.
PALABRAS CLAVE: hiperparatiroidismo; paratiroides; PET colina; gammagrafía MIBI; fluorocolina
INTRODUCTION
The location of the pathological parathyroid glands in hyperparathyroidism is usually performed by SPECT/TC scan with 99mTc-sestamibi (MIBI) which increases their accuracy when associating ultrasound scanning. The non-location of the parathyroid glands increases difficulties for surgical removal. Other radioactive tracers such as methionine or fluorocholine are used to increase the detection of pathological glands [1–8].
The usefulness of PET/TC with 18-Fluorocholine (CH) was established after incidental findings of pathological parathyroid in males tracking for prostate cancer. In 2012 Mapelli et al., in 2013 Quak et al. and, in 2014 Hodolic et al. described cases of incidental uptake in parathyroids in explorations with F-18-fluorocholine in males with prostate cancer and proposed it as a study in case of negative MIBI [9–11]. Subsequent studies have confirmed this indication [12–14].
The accuracy of nuclear scans in the location of pathological parathyroid glands in hyperparathyroidism has been widely published and debated in the literature and the absence of localization poses a greater difficulty in surgical treatment so research is continued to establish a diagnostic strategy that offers the highest number of true positives and fewer false negatives.
The objective of this review is to know whether PET/TC with 18-Fluorocholine in patients with hyperparathyroidism increases the number of catches compared to the scan with 99mTc-MIBI by bibliographic review.
METHOD
The following research PICO question was asked: In patients with primary hyperparathyroidism [patient] the location of the pathological glands [intervention] by PET/TC with 18-Fluorocholine (CH) versus SPECT/TC with 99mTc-MIBI (MIBI) [comparison] does it offer more detections with suspected pathology? [outcome].
Systematic review in the PubMed (https://pubmed.ncbi.nlm.nih.gov/), WoS (http://wos.fecyt.es/), ClinicalTrials (https://clinicaltrials.gov/) and Cochrahe (https://www.cochranelibrary.com/) databases with closure on December 17, 2019 following the guidelines of the PRISMA group [15] and Cochrane method [16] with the search descriptors and strategies summarized in Figure 1.
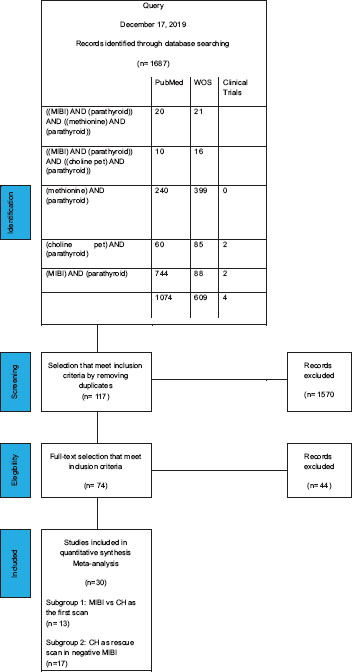
Figure 1. Bibliographical search and literature selection strategies.
Inclusion criteria: studies including patients with hyperparathyroidism undergoing scan with 99mTc-Sesta-MIBI (MIBI) and 18F-choline PET/CT (CH) as first scan (subgroup 1) and patients with study 99mTc-Sesta-MIBI (MIBI) negative in the first scan to be performed second rescue scan with 18F-choline PET/CT (CH) in which there was at least a significant scan uptake (subgroup 2). Articles indicating the number of patients scanned and the number of patients in whom there was at least a positive uptake in the neck or mediastinum and those in which there was no uptake or this nor was conclusive evaluated with SUVmax measurement (maximum standardized absorption value).
Exclusion criteria: clinical cases, conferences, conferences with published data or parathyroid cancer series exclusively.
Each article obtained the total number of patients with scans performed and calculated the prevalence of patients in which there was at least one uptake (positive uptake) or there was no uptake, or this was doubtful (negative uptake).
Two subgroups were analyzed:
Subgroup 1: essays comparing both techniques (CH vs. MIBI) as an initial scan.
Meta-analysis of dicotomical models was performed following the random effects model, the odds ratio and the publication bias were calculated.
Subgroup 2: studies that include CH as a rescue scan in patients with prior negative study with MIBI scan.
Meta-analysis of the prevalence of the number of patients in which there was at least one uptake was performed using the random effects model and the publication bias was evaluated.
The statistical program JAMOVI 1.2.22 (The jamovi project 2020, https://www.jamovi.org) was used.
STUDY LIMITATIONS
• Only patients where at least one scan uptake was detected.
• The number of uptakes per patient was not evaluated.
• Patients with primary hyperparathyroidism are included but in some cases the diagnosis is not clear.
• Correlation of catchments with surgical findings was not sought to assess the accuracy of the tests.
• It is assumed that the scan uptake increases the probability of surgical location.
RESULTS
SUBGROUP 1
13 studies including 1131 scans (596 PET/TC with 18-Fluorocholine vs. 535 SPECT/TC scan with 99mTc-sestamibi) [14,17–28] were selected. See Table 1.
Table 1. Subgroup 1: MIBI vs CH as the first scan. Results table.
|
CH PET/TC |
|
|
99mTc-sestamibi SPECT/CT |
|
|
study name |
N |
CAPTURES |
NO CAPTURE |
N |
CAPTURES |
NO CAPTURE |
Thansser 2017 [17] |
54 |
52 |
2 |
54 |
42 |
12 |
Orevi 2014 [21] |
40 |
37 |
3 |
40 |
33 |
7 |
Beheshti 2018 [22] |
82 |
76 |
6 |
82 |
50 |
32 |
Araz 2018 [24] |
35 |
30 |
5 |
35 |
28 |
7 |
Bossert 2019 [25] |
34 |
24 |
10 |
34 |
5 |
29 |
Araz 2018 2 [23] |
43 |
42 |
1 |
43 |
35 |
8 |
Imamovic 2016 [26] |
41 |
39 |
2 |
41 |
27 |
14 |
Hocevar 2017 [27] |
151 |
126 |
25 |
90 |
74 |
16 |
Kluijfhout 2016 [28] |
44 |
34 |
10 |
44 |
14 |
30 |
Michaud 2015 [14] |
17 |
15 |
2 |
17 |
15 |
2 |
Khafif 2019 [19] |
19 |
16 |
3 |
19 |
14 |
5 |
Lezaic 2014 [20] |
24 |
24 |
0 |
24 |
20 |
4 |
Michaud 2014 [18] |
12 |
11 |
1 |
12 |
7 |
5 |
|
596 |
526 |
70 |
535 |
364 |
171 |
The number of patients with at least one uptake is significantly higher with 18-Fluorocholine scans (OR 4,264, CI 95% 2,400-7,577). The prevalence of uptakes with 18-Fluorocholine is 0.91 [0.86, 0.95] and with MIBI of 0.68 [0.56, 0.80]. See Figure 2 and Table 2.
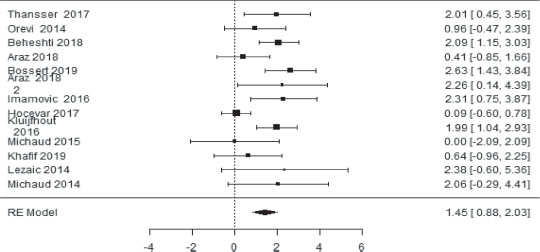
Figure 2. Subgroup 1: MIBI vs CH as the first scan. Forest plot.
Table 2. Statistical heterogeneity.
Random-Effects Model (k =13) |
||||||
|
Estimate |
se |
z |
p |
Cl Lower Bound |
Cl Upper Bound |
Intercept |
1.45 |
0.293 |
4.95 |
<.001 |
0.875 |
2.025 |
|
. |
. |
. |
. |
. |
. |
Note. Tau2 Estimator: Restricted Maximum-Likelihood
Heterogeneity Statistics |
|||||||
Tau |
Tau2 |
I2 |
H2 |
R2 |
df |
Q |
p |
0.742 |
0.5498 (SE= 0.4357) |
55.35% |
2.239 |
. |
12.000 |
29.741 |
0.003 |
Back-Transform Log Odds Ratio to Odds Ratioo Odds Ratio |
||
Odds Ratio |
Cl Lower Bound |
CI Upper Bound |
4.264 |
2.400 |
7.577 |
Robust Paired Samples-T-Test |
|||||||||
|
|
t |
df |
p |
Mean difference |
SE |
95% Confidence Interval |
||
Lower |
Upper |
Cohen’s d |
|||||||
CAPTA_CH |
CAPTA_MIBI |
3.49 |
8.00 |
0.008 |
7.78 |
2.23 |
2.63 |
12.922 |
0.317 |
NOCAPTA_CH |
NOCAPTA_MIBI |
−2.60 |
8.00 |
0.032 |
−7.67 |
2.95 |
−14.48 |
−0.858 |
0.731 |
The publication bias is moderate (I2-55.35%). See Figure 3.
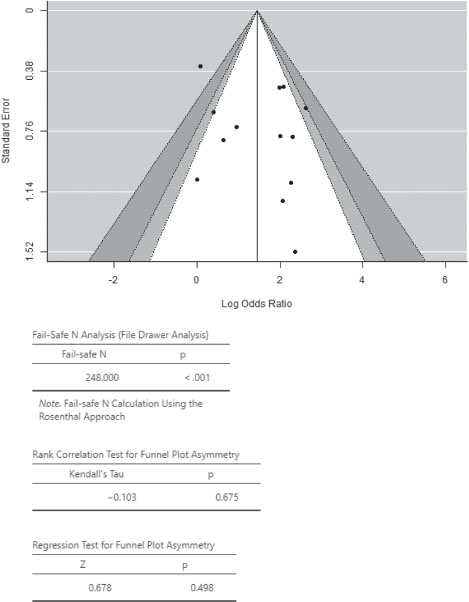
Figure 3. Subgroup 1: MIBI vs CH as the first scan. Funnel plot and publication bias
SUBGROUP 2
17 articles including 412 scans were selected with at least 359 patients in which there was at least one uptake [17,21,23,29–41]. See Table 3.
Table 3. Subgroup 2: CH as a rescue scan in negative MIBI. Results table.
Study name |
N |
CAPTURES |
NO CAPTURE |
Piccardo 2019 [35] |
44 |
32 |
12 |
Thansser 2017 [17] |
11 |
11 |
0 |
Orevi 2014 [21] |
7 |
7 |
0 |
Zajickova 2018 [36] |
13 |
12 |
1 |
Kluijfhout 2017 [37] |
10 |
9 |
1 |
Quak 2018 [38] |
25 |
22 |
3 |
Morales 2018 [39] |
49 |
42 |
7 |
Bera 2018 [40] |
29 |
26 |
3 |
Amadou 2019 [41] |
29 |
28 |
1 |
Liu 2019 [29] |
87 |
70 |
17 |
Christakis 2019 [30] |
12 |
12 |
0 |
Collaud 2019 [31] |
7 |
6 |
1 |
Grimaldi 2018 [32] |
27 |
24 |
3 |
Huber 2018 [33] |
26 |
25 |
1 |
Kluijfhout 2015 [37] |
5 |
4 |
1 |
Treglia 2016 [34] |
23 |
21 |
2 |
Araz 2018 2 [23] |
8 |
8 |
0 |
|
412 |
359 |
53 |
The prevalence of uptakes among patients with prior negative MIBI studies was 0.90 [0.87, 0.94]. The probability of detection of both techniques in this group reaches 0.98. See Figure 4 and Table 4.
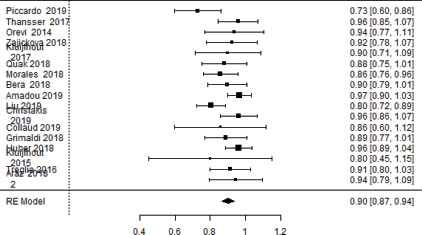
Figure 4. Subgroup 2: CH as a rescue scan in negative MIBI. Forest plot.
Table 4. Statistical heterogeneity.
Random-Effects Model (k = 17)= 17) |
||||||
|
Estimate |
se |
Z |
p |
Cl Lower Bound |
Cl Upper Bound |
Intercept |
0.902 |
0.0181 |
49.7 |
< .001 |
0.867 |
0.938 |
|
. |
. |
. |
. |
. |
. |
Note. Tau2 Estimator: Restricted Maximum-Likelihood
Heterogeneity Statistics |
|||||||
Tau |
Tau2 |
I2 |
H2 |
R2 |
df |
Q |
p |
0.042 |
0.0018 (SE= 0.0018) |
34.5% |
1.527 |
. |
16.000 |
22.101 |
0.140 |
Random-Effects Model (k = 17) |
||||||
|
Estimate |
se |
Z |
p |
CI Lower Bound |
CI Upper Bound |
Intercept |
0.902 |
0.0181 |
49.7 |
< .001 |
0.867 |
0.938 |
|
. |
. |
. |
. |
. |
. |
Note. Tau2 Estimator: Restricted Maximum-Likelihood
Heterogeneity Statistics |
|||||||
Tau |
Tau2 |
I2 |
H2 |
R2 |
df |
Q |
p |
0.042 |
0.0018 (SE= 0.0018) |
34.5% |
1.527 |
. |
16.000 |
22.101 |
0.140 |
The publication bias in meta-analysis is low (I2-34.5%). See Figure 5.
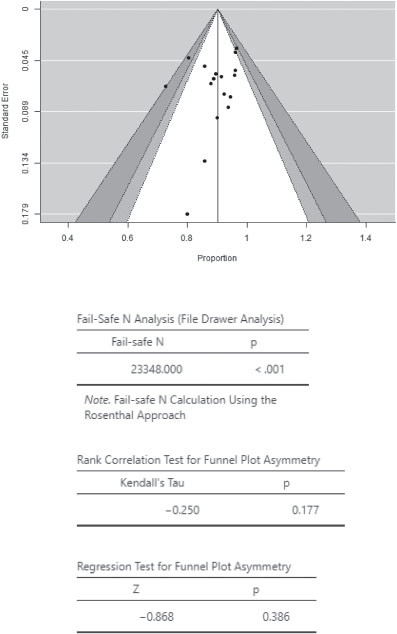
Figure 5. Subgroup 2: CH as a rescue scan in negative MIBI. Funnel plot and publishing bias.
DISCUSSION
Currently, the definitive treatment of hyperparathyroidism is the surgical removal of the gland or pathological glands. Negative localization studies make surgical treatment difficult.
In both the selected articles in our meta-analysis and in previous meta-analysis, CH localization studies have shown greater ability to locate pathological glands [34,42–45] than MIBI or methionine [46–48] in both first exploration and rescue scan [31,49].
The probability of uptake with CH is above 0.9 on both first scans and scans performed after negative MIBI study (in these cases the combination of both techniques reaches a prevalence of uptake of 0.97). See Figure 6.
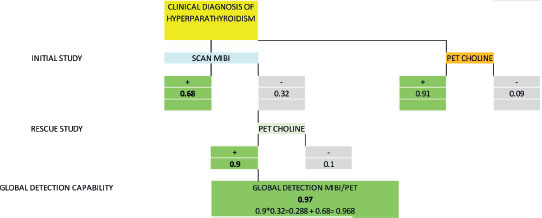
Figure 6. Prevalence of uptake with SPECT/TC-MIBI and PET/TC-Choline in hyperparathyroidism.
The CH localization study using PET/TC offers advantages such as higher number of uptakes (both the number of patients with at least one uptake and the higher number of multiple adenoma or hyperplasia captures [20], shorter imaging time [14] and exposure of patients with less radiation than the SPECT/CT hybrid image with Tc-99m-sestaMIBI [50].
As disadvantages is the difficulty in distinguishing catches in thyroid, nodes, thymus or muscle (false positives) [50] and logistical problems [14].
CH scan may be indicated both as an initial scan and in patients with prior negative MIBI study.
CONCLUSIONS
1. Ultrasound-associated SPECT/TC-MIBI scan is currently the scan of choice for the location of pathological parathyroid glands prior to surgery.
2. PET-Choline scan increases the number of patients with at least one uptake on both the first scan and on scans with initial negative MIBI studies.
3. Currently PET-Choline scan seems an option to locate pathological glands in patients with negative initial scan.
REFERENCES
1.Hindié E, Zanotti-Fregonara P, Tabarin A, Rubello D, Morelec I, Wagner T, et al. The role of radionuclide imaging in the surgical management of primary hyperparathyroidism. J Nucl Med. 2015 May 1;56(5):737-44. https://doi.org/10.2967/jnumed.115.156018
2.Lussey-Lepoutre C, Trésallet C, Ghander C, Morelec I, Najah H, Kasereka-kisenge F, et al. Rôle de l'imagerie dans le bilan préopératoire des hyperparathyroïdies primaires. Med Nucl. 2018 Jan 1;42(1):49-58. https://doi.org/10.1016/j.mednuc.2017.12.001
3.Prior JO. New scintigraphic methods for parathyroid imaging. Ann Endocrinol (Paris). 2015 May 1;76(2):145-7. https://doi.org/10.1016/j.ando.2015.03.026
4.Weber T, Luster M. C-11-Methionin-PET/CT zur Lokalisation von Nebenschilddrüsenadenomen. Vol. 85, Chirurg. Springer Verlag; 2014. p. 601-6. https://doi.org/10.1007/s00104-013-2695-5
5.Grassetto G, Alavi A, Rubello D. PET and Parathyroid. Vol. 2, PET Clinics. 2007. p. 385-93. https://doi.org/10.1016/j.cpet.2008.04.005
6.Kettle AG, O'Doherty MJ. Parathyroid Imaging: How Good Is It and How Should It Be Done? Semin Nucl Med. 2006 Jul;36(3):206-11. https://doi.org/10.1053/j.semnuclmed.2006.03.003
7.Imperiale A, Taïeb D, Hindié E. 18 F-Fluorocholine PET/CT as a second line nuclear imaging technique before surgery for primary hyperparathyroidism. Vol. 45, European Journal of Nuclear Medicine and Molecular Imaging. Springer Berlin Heidelberg; 2018. p. 654-7. https://doi.org/10.1007/s00259-017-3920-0
8.García-Talavera San Miguel P, Gómez-Caminero López F, Villanueva Curto JG, Tamayo Alonso MP, Martín Gómez ME. Update of the role of Nuclear Medicine techniques in the pre-surgical localization of primary hyperparathyroidism. Rev Esp Med Nucl Imagen Mol. 2019 Mar 1;38(2):123-35. https://doi.org/10.1016/j.remnie.2019.01.006
9.Mapelli P, Busnardo E, Magnani P, Freschi M, Picchio M, Gianolli L, et al. Incidental finding of parathyroid adenoma with 11C-choline PET/CT. Clin Nucl Med. 2012 Jun;37(6):593-5. https://doi.org/10.1097/RLU.0b013e31824c5ffc
10. Quak E, Lheureux S, Reznik Y, Bardet S, Aide N. F18-choline, a novel PET tracer for parathyroid adenoma? Vol. 98, Journal of Clinical Endocrinology and Metabolism. 2013. p. 3111-2. https://doi.org/10.1210/jc.2013-2084
11. Hodolic M, Huchet V, Balogova S, Michaud L, Kerrou K, Nataf V, et al. Incidental uptake of 18F-fluorocholine (FCH) in the head or in the neck of patients with prostate cancer. Radiol Oncol. 2014 Sep 1;48(3):228-34. https://doi.org/10.2478/raon-2013-0075
12. Parvinian A, Martin-Macintosh EL, Goenka AH, Durski JM, Mullan BP, Kemp BJ, et al. 11C-choline PET/CT for detection and localization of parathyroid adenomas. Am J Roentgenol. 2018 Feb 1;210(2):418-22. https://doi.org/10.2214/AJR.17.18312
13. Kluijfhout WP, Vorselaars WMCM, Vriens MR, Borel Rinkes IHM, Valk GD, De Keizer B. Enabling minimal invasive parathyroidectomy for patients with primary hyperparathyroidism using Tc-99m-sestamibi SPECT-CT, ultrasound and first results of 18F-fluorocholine PET-CT. Eur J Radiol. 2015 Sep 1;84(9):1745-51. https://doi.org/10.1016/j.ejrad.2015.05.024
14. Michaud L, Balogova S, Burgess A, Ohnona J, Huchet V, Kerrou K, et al. A pilot comparison of 18F-fluorocholine PET/CT, ultrasonography and 123I/99mTc-sestaMIBI dual-phase dual-isotope scintigraphy in the preoperative localization of hyperfunctioning parathyroid glands in primary or secondary hyperparathyroidism: Influence of. Med (United States). 2015;94(41). https://doi.org/10.1097/MD.0000000000001701
15. Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015 Jan 2;350:g7647. https://doi.org/10.1136/bmj.g7647
16. Centro Cochrane Iberoamericano traductores. Manual Cochrane de Revisiones Sistemáticas de Intervenciones, versión 5.1.0 [actualizada en marzo de 2011]. Barcelona; 2012. 639 p.
17. Thanseer N, Bhadada SK, Sood A, Mittal BR, Behera A, Gorla AKR, et al. Comparative Effectiveness of Ultrasonography, 99mTc-Sestamibi, and 18F-Fluorocholine PET/CT in Detecting Parathyroid Adenomas in Patients With Primary Hyperparathyroidism. Clin Nucl Med. 2017;42(12):e491-7. https://doi.org/10.1097/RLU.0000000000001845
18. Michaud L, Burgess A, Huchet V, Lefèvre M, Tassart M, Ohnona J, et al. Is 18F-fluorocholine-positron emission tomography/ computerized tomography a new imaging tool for detecting hyperfunctioning parathyroid glands in primary or secondary hyperparathyroidism? J Clin Endocrinol Metab. 2014 Dec 1;99(12):4531-6. https://doi.org/10.1210/jc.2014-2821
19. Khafif A, Masalha M, Landsberg R, Domachevsky L, Bernstine H, Groshar D, et al. The role of F18-fluorocholine positron emission tomography/magnetic resonance imaging in localizing parathyroid adenomas. Eur Arch Oto-Rhino-Laryngology. 2019;276(5):1509-16. https://doi.org/10.1007/s00405-019-05301-2
20. Lezaic L, Rep S, Sever MJ, Kocjan T, Hocevar M, Fettich J. 18F-Fluorocholine PET/CT for localization of hyperfunctioning parathyroid tissue in primary hyperparathyroidism: a pilot study. Eur J Nucl Med Mol Imaging. 2014;41(11):2083-9. https://doi.org/10.1007/s00259-014-2837-0
21. Orevi M, Freedman N, Mishani E, Bocher M, Jacobson O, Krausz Y. Localization of parathyroid adenoma by 11C-Choline PET/CT preliminary results. Clin Nucl Med. 2014;39(12):1033-8. https://doi.org/10.1097/RLU.0000000000000607
22. Beheshti M, Hehenwarter L, Paymani Z, Rendl G, Imamovic L, Rettenbacher R, et al. 18F-Fluorocholine PET/CT in the assessment of primary hyperparathyroidism compared with 99mTc-MIBI or 99mTc-tetrofosmin SPECT/CT: a prospective dual-centre study in 100 patients. Eur J Nucl Med Mol Imaging. 2018 Sep 1;45(10):1762-71. https://doi.org/10.1007/s00259-018-3980-9
23. Araz, C. Soydal, E. Ozkan, M. Kir, E. İbis, S. Gullu MF, Erdogan, R. Emral ONK. The Efficacy of 18F Choline PET/CT in comparison to Tc99m MIBI SPECT/CT in the Localisation of Hyperfunctioning Parathyroid Gland in primary Hyperparathyroidism. Eur J Nucl Med Mol Imaging. 2018;45(Suppl. 1):S89-90. https://doi.org/10.1097/MNM.0000000000000899
24. Araz M, Soydal Ç, Özkan E, Kır MK, İbiş E, Güllü S, et al. The efficacy of fluorine-18-choline PET/CT in comparison with 99mTc-MIBI SPECT/CT in the localization of a hyperfunctioning parathyroid gland in primary hyperparathyroidism. Nucl Med Commun. 2018;39(11):989-94. https://doi.org/10.1097/MNM.0000000000000899
25. Bossert I, Chytiris S, Hodolic M, Croce L, Mansi L, Chiovato L, et al. PETC/CT with 18 F-Choline localizes hyperfunctioning parathyroid adenomas equally well in normocalcemic hyperparathyroidism as in overt hyperparathyroidism. J Endocrinol Invest. 2019 Apr 2;42(4):419-26. https://doi.org/10.1007/s40618-018-0931-z
26. Imamovic L. F18 Choline PET-CT: an accurate diagnostic tool for the detection of parathyroid adenoma? Mol imaging Biol Conf world Mol imaging Congr 2016 United states Conf start 20160907 Conf end 20160910. 2016;(2 Supplement).
27. Hocevar M, Lezaic L, Rep S, Zaletel K, Kocjan T, Sever MJ, et al. Focused parathyroidectomy without intraoperative parathormone testing is safe after pre-operative localization with 18F-Fluorocholine PET/CT. Eur J Surg Oncol. 2017 Jan 1;43(1):133-7. https://doi.org/10.1016/j.ejso.2016.09.016
28. Kluijfhout WP, Vorselaars WMCM, Van Den Berk SAM, Vriens MR, Borel Rinkes IHM, Valk GD, et al. Fluorine-18 fluorocholine PET-CT localizes hyperparathyroidism in patients with inconclusive conventional imaging: A multicenter study from the Netherlands. Nucl Med Commun. 2016 Nov 1;37(12):1246-52. https://doi.org/10.1097/MNM.0000000000000595
29. Liu Y, Dang Y, Huo L, Hu Y, Wang O, Liu H, et al. Preoperative localisation of adenomas in primary hyperparathyroidism: the value of 11 C-choline PET/CT in patients with negative or discordant ultrasonography and 99m Tc-Sesta-MIBI-SPECT/CT. J Nucl Med. 2019 Oct 10;jnumed.119.233213. https://doi.org/10.2967/jnumed.119.233213
30. Christakis I, Khan S, Sadler GP, Gleeson F V., Bradley KM, Mihai R. 18Fluorocholine PET/CT scanning with arterial phase-enhanced CT is useful for persistent/ recurrent primary hyperparathyroidism: First UK case series results. In: Annals of the Royal College of Surgeons of England. Royal College of Surgeons of England; 2019. p. 501-7. https://doi.org/10.1308/rcsann.2019.0059
31. Boccalatte LA, Higuera F, Gómez NL, De La Torre AY, Mazzaro EL, Galich AM, et al. Usefulness of 18F-fluorocholine positron emission tomography-computed tomography in locating lesions in hyperparathyroidism: A systematic review. Vol. 145, JAMA Otolaryngology - Head and Neck Surgery. American Medical Association; 2019. p. 743-50. https://doi.org/10.1001/jamaoto.2019.0574
32. Grimaldi S, Young J, Kamenicky P, Hartl D, Terroir M, Leboulleux S, et al. Challenging pre-surgical localization of hyperfunctioning parathyroid glands in primary hyperparathyroidism: the added value of 18F-Fluorocholine PET/CT. Eur J Nucl Med Mol Imaging. 2018 Sep 1;45(10):1772-80. https://doi.org/10.1007/s00259-018-4018-z
33. Huber GF, Hüllner M, Schmid C, Brunner A, Sah B, Vetter D, et al. Benefit of 18 F-fluorocholine PET imaging in parathyroid surgery. Vol. 28, European Radiology. Springer Verlag; 2018. p. 2700-7. https://doi.org/10.1007/s00330-017-5190-4
34. Treglia G, Sadeghi R, Schalin-Jäntti C, Caldarella C, Ceriani L, Giovanella L. Detection rate of 99mTc-MIBI single photon emission computed tomography (SPECT)/CT in preoperative planning for patients with primary hyperparathyroidism: A meta-analysis. Vol. 38, Head and Neck. John Wiley and Sons Inc.; 2016. p. E2159-72. https://doi.org/10.1002/hed.24027
35. Piccardo A, Trimboli P, Rutigliani M, Puntoni M, Foppiani L, Bacigalupo L, et al. Additional value of integrated 18 F-choline PET/4D contrast-enhanced CT in the localization of hyperfunctioning parathyroid glands and correlation with molecular profile. Eur J Nucl Med Mol Imaging. 2019;46(3):766-75. https://doi.org/10.1007/s00259-018-4147-4
36. Zajickova, K; Zogala, D; Kubinyi J. Parathyroid Imaging by 18F-Fluorocholine PET/CT in Patients With Primary Hyperparathyroidism and Inconclusive Conventional Methods: Clinico-Pathological Correlations. Physiol Res. 2018 Nov 30;S551-7. https://doi.org/10.33549/physiolres.934029
37. Kluijfhout WP, Pasternak JD, Gosnell JE, Shen WT, Duh QY, Vriens MR, et al. 18F fluorocholine PET/MR imaging in patients with primary hyperparathyroidism and inconclusive conventional imaging: A prospective pilot study. Radiology. 2017 Aug 1;284(2):460-7. https://doi.org/10.1148/radiol.2016160768
38. Quak E, Blanchard D, Houdu B, Le Roux Y, Ciappuccini R, Lireux B, et al. F18-choline PET/CT guided surgery in primary hyperparathyroidism when ultrasound and MIBI SPECT/CT are negative or inconclusive: the APACH1 study. Eur J Nucl Med Mol Imaging. 2018 Apr 1;45(4):658-66. https://doi.org/10.1007/s00259-017-3911-1
39. M. I. Morales-Lozano, C. Perdomo1, F. Grisanti1, O. Ajuria J, Rosales, C. Silva JA. Primary hyperparathyroidism and negative conventional imaging: value of 11C-Methionine PET/CT and comparison with 11C-Choline PET/CT. Eur J Nucl Med Mol Imaging. 2018;45(Suppl. 1):S88-9.
40. G. Bera, C. Amadou, M. Ezziane, L. Chami, T. Delbot, A. Rouxel M, Leban, G. Herve, F. Menegaux, L. Leenhardt, A. Kas, C. Tresalet C, Ghander CL-L. 18F-fluorocholine PET/CT and parathyroid 4D Computed Tomography: First results of an alternative and efficient imaging tool in reoperative patients with primary hyperparathyroidism. Eur J Nucl Med Mol Imaging. 2018;45(Suppl. 1):S90.
41. Amadou C, Bera G, Ezziane M, Chami L, Delbot T, Rouxel A, et al. 18F-Fluorocholine PET/CT and Parathyroid 4D Computed Tomography for Primary Hyperparathyroidism: The Challenge of Reoperative Patients. World J Surg. 2019 May 15;43(5):1232-42. https://doi.org/10.1007/s00268-019-04910-6
42. Treglia G, Piccardo A, Imperiale A, Strobel K, Kaufmann PA, Prior JO, et al. Diagnostic performance of choline PET for detection of hyperfunctioning parathyroid glands in hyperparathyroidism: a systematic review and meta-analysis. Eur J Nucl Med Mol Imaging. 2019;46(3):751-65. https://doi.org/10.1007/s00259-018-4123-z
43. Kim SJ, Lee SW, Jeong SY, Pak K, Kim K. Diagnostic Performance of F-18 Fluorocholine PET/CT for Parathyroid Localization in Hyperparathyroidism: a Systematic Review and Meta-Analysis. Horm Cancer. 2018;9(6):440-7. https://doi.org/10.1007/s12672-018-0347-4
44. Treglia G, Trimboli P, Huellner M, Giovanella L. Imaging in primary hyperparathyroidism: Focus on the evidence-based diagnostic performance of different methods. Vol. 43, Minerva Endocrinologica. Edizioni Minerva Medica; 2018. p. 133-43. https://doi.org/10.23736/S0391-1977.17.02685-2
45. Broos WAM, Wondergem M, Knol RJJ, van der Zant FM. Parathyroid imaging with 18F-fluorocholine PET/CT as a first-line imaging modality in primary hyperparathyroidism: a retrospective cohort study. EJNMMI Res. 2019 Dec 1;9(1). https://doi.org/10.1186/s13550-019-0544-3
46. Kluijfhout WP, Pasternak JD, Drake FT, Beninato T, Gosnell JE, Shen WT, et al. Use of PET tracers for parathyroid localization: a systematic review and meta-analysis. Langenbeck's Arch Surg. 2016 Nov 1;401(7):925-35. https://doi.org/10.1007/s00423-016-1425-0
47. Yuan L, Liu J, Kan Y, Yang J, Wang X. The diagnostic value of 11C-methionine PET in hyperparathyroidism with negative 99mTc-MIBI SPECT: A meta-analysis. Vol. 58, Acta Radiologica. SAGE Publications Inc.; 2017. p. 558-64. https://doi.org/10.1177/0284185116661878
48. Caldarella C, Treglia G, Isgrò MA, Giordano A. Diagnostic performance of positron emission tomography using 11C-methionine in patients with suspected parathyroid adenoma: A meta-analysis. Endocrine. 2013 Feb;43(1):78-83. https://doi.org/10.1007/s12020-012-9746-4
49. Broos WAM, Van Der Zant FM, Knol RJJ, Wondergem M. Choline PET/CT in parathyroid imaging: a systematic review. Vol. 40, Nuclear Medicine Communications. Lippincott Williams and Wilkins; 2019. p. 96-105. https://doi.org/10.1097/MNM.0000000000000952
50. Rep S, Hocevar M, Vaupotic J, Zdesar U, Zaletel K, Lezaic L. 18F-choline PET/CT for parathyroid scintigraphy: Significantly lower radiation exposure of patients in comparison to conventional nuclear medicine imaging approaches. J Radiol Prot. 2018 Mar 1;38(1):343-56. https://doi.org/10.1088/1361-6498/aaa86f